HIPAA Compliant
•
SOC 2 Type II Certified
•
ISO 9001 Certified
•
ISO 27001 Certified
•
GDPR Compliant
Our client is a New York based insurance provider, managing life and disability insurance policies. Their underwriting and claims teams heavily relied on Attending Physician Statements to their processes. Whether to assess medical risks, validate disclosures, and make accurate policy decisions, they needed a thorough review of APS records. These reviews directly impacted policy issuance timelines, claim closures, and overall operational costs.
With growing application volumes, APS processes had become a critical pressure for their team.
Even with experienced underwriters and adjusters, their APS process was slow, costly, and difficult to scale.
They faced repeated issues with their existing APS process:
As APS case volumes increased, the client had two choices, either to hire more staff or find a smarter, automated approach.
We identified that the major issue was not with APS record retrieval but with the way the APS records were processed, organized, and delivered to the decision-makers.
We designed a solution combining AI-automation of APS processes with medical expert supervision to provide clear, organized APS summaries that reduced manual efforts and operational costs for them.
See what we did for them:
We worked with the underwriting and claims teams to understand their processes like:
Based on these, we designed a custom APS summary process aligned with their underwriting and claims requirements.
We implemented a hybrid APS review process where:
This ensured faster turnaround without compromising quality and medical reliability.
The impact of this AI-driven APS model was immediate and measurable.

Our AI system processed large volumes of APS records, extracting key insurance-related information such as:
This removed hours of manual review per case.
We delivered APS summaries in a clean, structured format. Underwriters could easily locate critical medical facts without shuffling through hundreds of pages.
AI systems flagged missing and unclear information, such as incomplete timelines or vague physician statements, early in the process. This reduced repeated follow-ups and eliminated additional rework.
Every APS summary was reviewed by trained medical professionals to ensure:
This reduced disputes and improved defensibility in underwriting and claims decisions.
Final APS summary reports were delivered in formats aligned with the client’s underwriting and claims systems, allowing teams to use them directly for their decision-making.
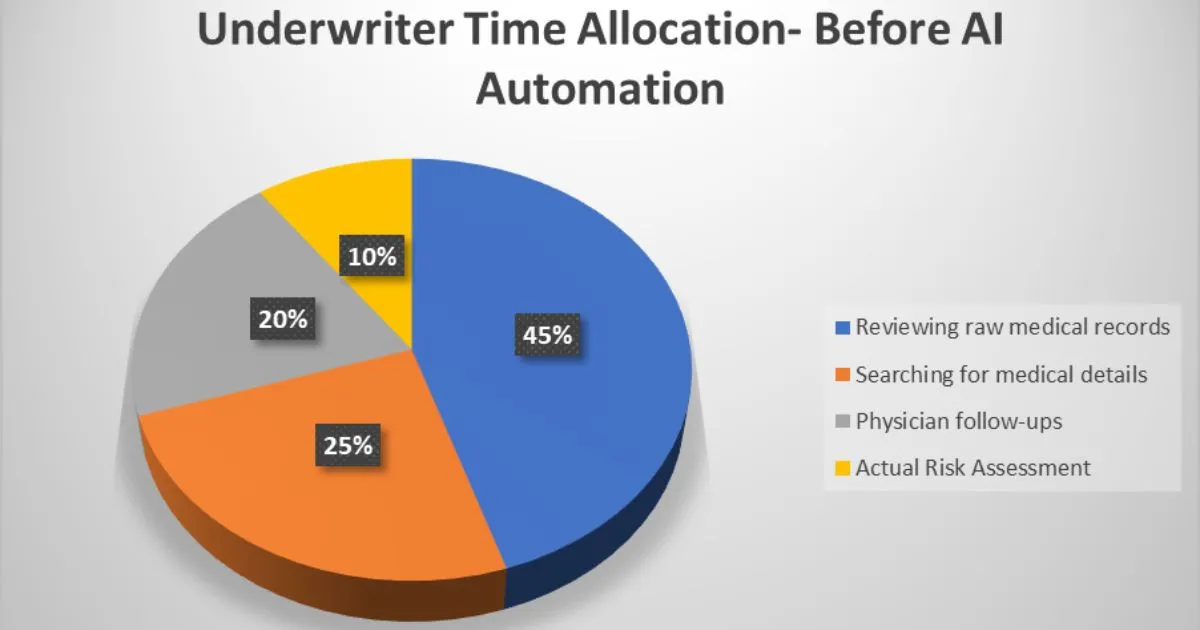
Before automation, underwriters and claims team spent most of their time on manual review and follow-ups rather than decision-making.
After implementing AI-driven APS automation, underwriter time shifted toward high-value risk assessment.
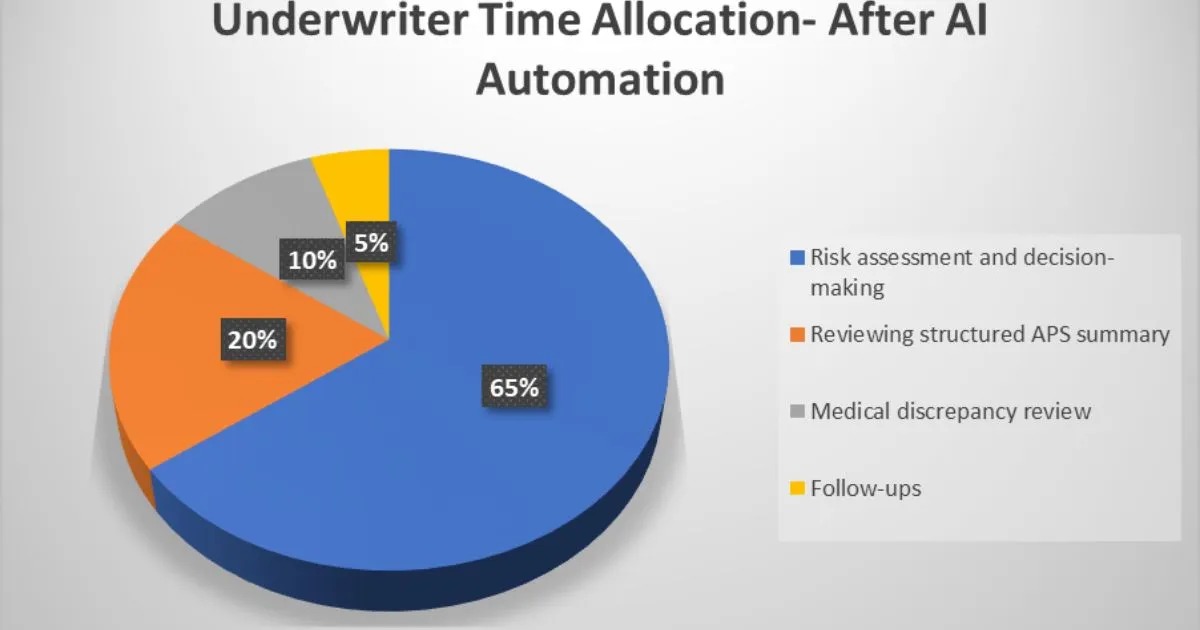
AI automation shifted underwriter effort away from administrative work towards faster and more confident decision-making.
Underwriters reclaimed 6–8 hours per week, allowing them to handle more cases without working overtime.
Within months, the client achieved a clear return on investment by lowering cost per APS while increasing decision-making capacity.
By combining APS process automation with medical expertise, we helped the client transform a slow and laborious APS process into a scalable and cost-efficient insurance claim support system. Underwriters and insurance adjusters gained faster access to clear medical insights, reduced operational costs, and made more consistent and defensible claim decisions.
“The structured APS summaries significantly reduced review time for our underwriting team. The clarity and consistency helped us make faster, more confident decisions while keeping costs under control.”
— Senior Underwriting Manager, Insurance Provider
Anjana Devi Vijay is a Medical–Legal Research Analyst with seven years of experience translating complex medical and legal information into clear, practical insights. Skilled in research, analytics, and deposition summary review, she understands the documentation and workflow challenges faced in the medical–legal field. She creates concise, solution-focused content-including blogs, eBooks, and case studies- that helps attorneys, evaluators, and claims professionals improve decision-making and strengthen case outcomes.